- 05 Apr 2024
- 1 Minute to read
- Print
- DarkLight
- PDF
SOAP 2.0 | Progress Notes
- Updated on 05 Apr 2024
- 1 Minute to read
- Print
- DarkLight
- PDF
Overview
Use Progress Notes to evaluate your patient as they progress through treatment. A Progress Note should be completed for Medicare patients after 9 Daily Notes.
There is no Progress Note requirement built into SOAP 2.0 for non-Medicare patients.
- A Progress Note will be required after 9 Daily Notes are finalized to comply with Medicare documentation requirements.
- The Daily Note option will be disabled until a Progress Note is finalized.
- Progress Notes that are marked as a re-certification must have updated Plan of Care dates with an end date in the future. Discover more about Medicare Plans of Care.
Click the arrow or colorblock below to discover more.
Progress Notes
SOAP 2.0 | Progress Notes
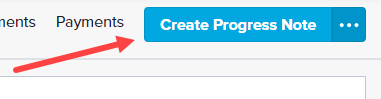
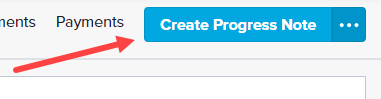
Click Create Progress Note. Your Progress Note type may be hiding in the (...) menu.
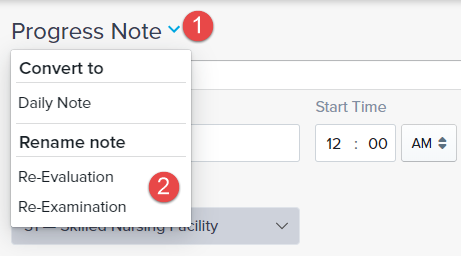
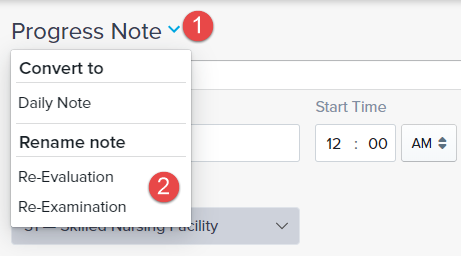
Progress Notes allow you to update the title of the note to comply with insurance requirements as needed. Discover more about Updating Progress Notes.
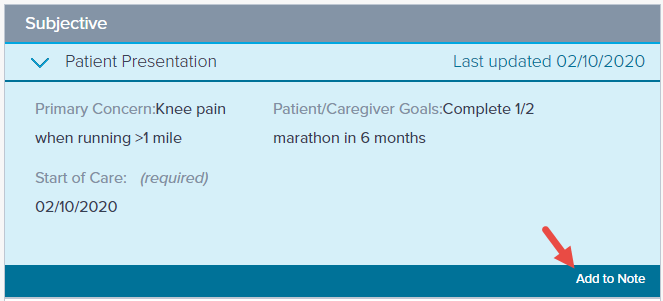
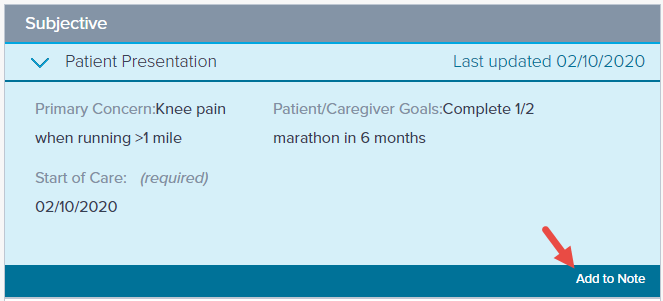
Similar to the Daily Note, you must edit the Patient Presentation subsection or click Add to Note.
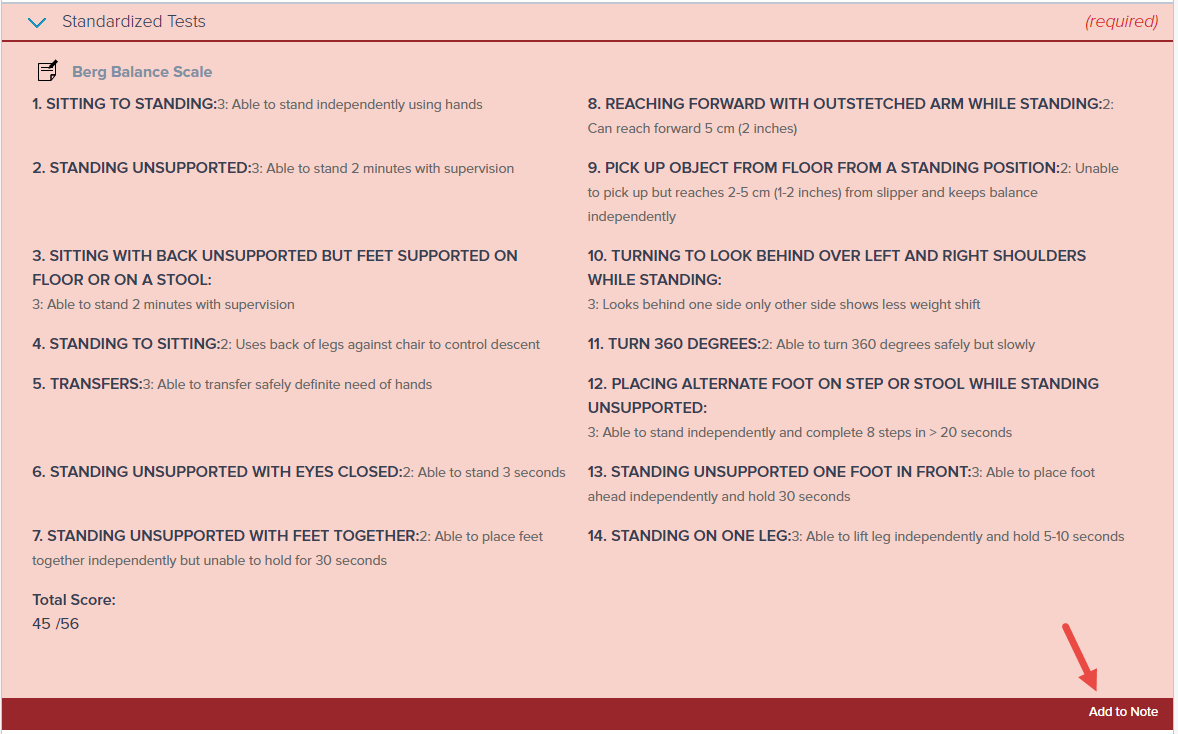
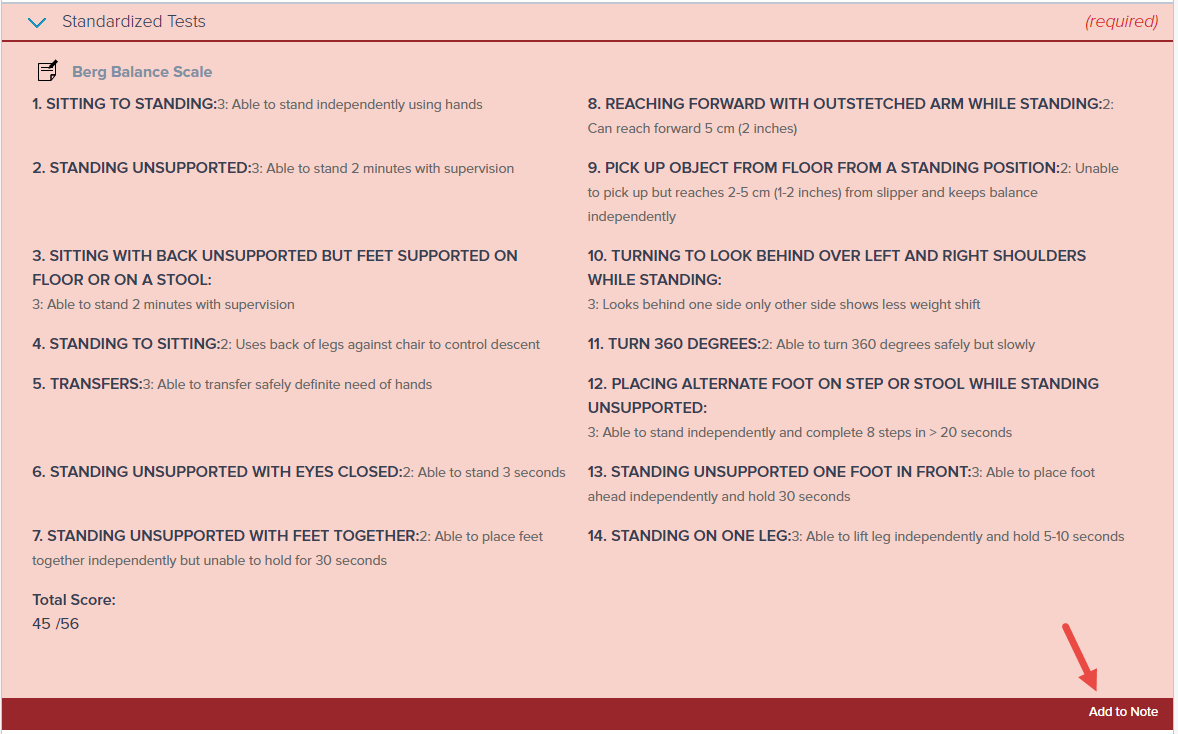
Medicare Patients: You’ll need to update your Standardized Test and the Plan of Care dates (if needed).
a. Re-administer the Standardized Test from the Objective section. Alternatively, you can click Add to Note.
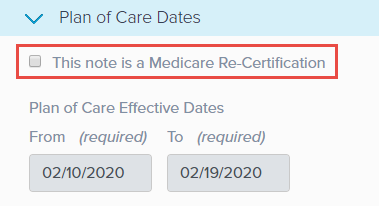
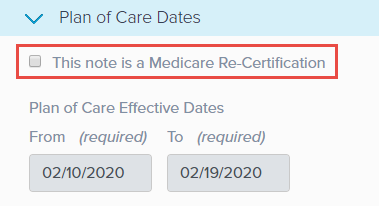
b. If you need to update the patient’s Plan of Care dates, start by navigating to the Plan of Care Dates subsection (Assessment).
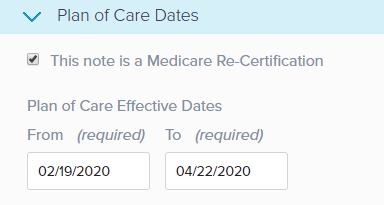
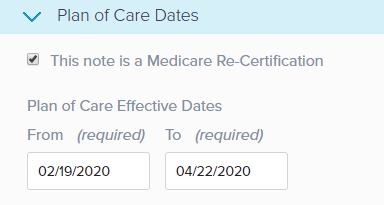
c. Check the This note is a medicare Re-Certification box.
d. This allows you to update the Plan of Care Effective Dates. The From date automatically updates to the current date and the To date is determined by the Duration selected in the Planned Treatment and Schedule subsection.
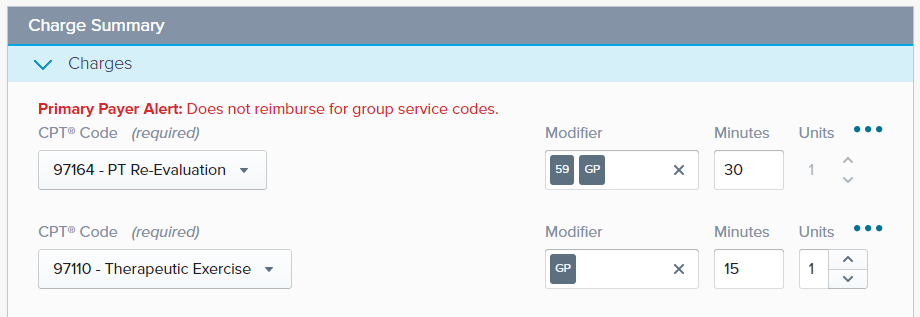
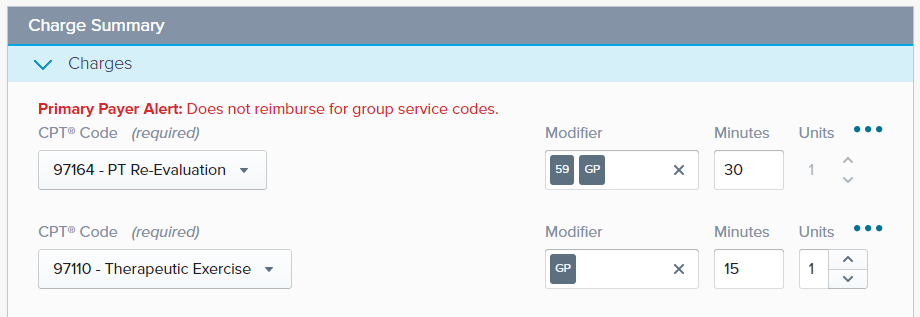
Click into the Charge Summary section to update the Minutes for our Timed Codes and add any additional codes like a Re-Eval code.
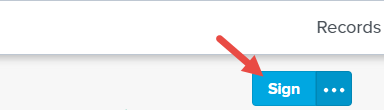
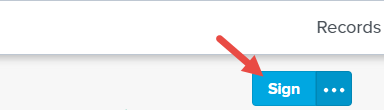
Click Sign when ready.